If you have a child or know an individual with a severe speech or language disorder, they may benefit from AAC. This is not just another acronym for you to remember, but rather the potential for your child to improve their communication skills with you and the world (or maybe just their next door neighbor; start small)!


So what is AAC?
AAC involves both augmentative and alternative communication, meaning it is a way to enhance one’s communication, i.e., augment, as well as an alternative means to communication. It can be as simple as a gesture (e.g. a thumbs up), or as complex as a high-tech computer that one controls with their eyes. Broadly speaking, it is often divided into three categories: no tech, low tech, and high tech.
Who needs AAC?
Individuals who may benefit from AAC include, but are not limited to, those with autism, down syndrome, apraxia, cerebral palsy, genetic/chromosomal differences, intellectual disability, degenerative disease, aphasia, or brain injury. AAC is not just for children; individuals of all ages with communication limitations may benefit from using AAC, no matter their prior history with or without it.
Just because your child may speak, or may be able to understand some language, does not mean that they would not benefit from AAC. Research supports the notion that speech and language skills continue to develop, potentially at a faster rate, with the use of AAC.

What does the speech-language pathologist (SLP) do?
The SLP is typically involved with evaluating, then recommending, if and what kind of AAC is appropriate for your child. They may provide strategies or recommendations for ways your child can communicate using AAC, both in and outside of therapy sessions. Depending on the situation, they may complete the funding/insurance requirements to provide a high tech device.
The SLP is typically involved with the implementation of the AAC system for your child. This means they work with your child to teach them how to use it for effective communication, as well as to continue to develop speech and language skills.
In some situations, there may be an AAC Specialist, who does the assessment and makes recommendations for your child, who is not their typical SLP. An AAC Specialist is typically an SLP whose primarily role is dedicated to AAC.
As a parent/caregiver, what do I do?
We are glad you asked! You want to be able to communicate effectively with your child, and your child wants to be able to communicate their wants/needs with you. Use the device and communication strategies that the SLP has recommended with your child. You may be able to join them for their sessions, or communicate with their SLP about specific recommendations. You are likely the one who communicates with your child the most, so you may also provide insight as to what is important to them and what is important to you to communicate. For example, if your child LOVES cheese puffs, having vocabulary to request cheese puffs would be important vocabulary to add to their device.
Exploring AAC for your child may seem overwhelming, but hopefully this article provided a little bit of insight about what it is and what it means. Do you have questions about a specific device or app? You are likely not the only one. We welcome you to comment below with your questions/feedback.
Want to learn more? We have many more posts that go into more detail about AAC!
Types of AAC Devices:
- No Tech AAC devices
- Low Tech AAC devices
- Mid Tech AAC devices, When to Use Mid Tech AAC
- High Tech AAC devices
- Dedicated AAC devices
Vocabulary, ownership, and use of AAC Devices:
- Operational competencies in AAC devices
- AAC System Ownership
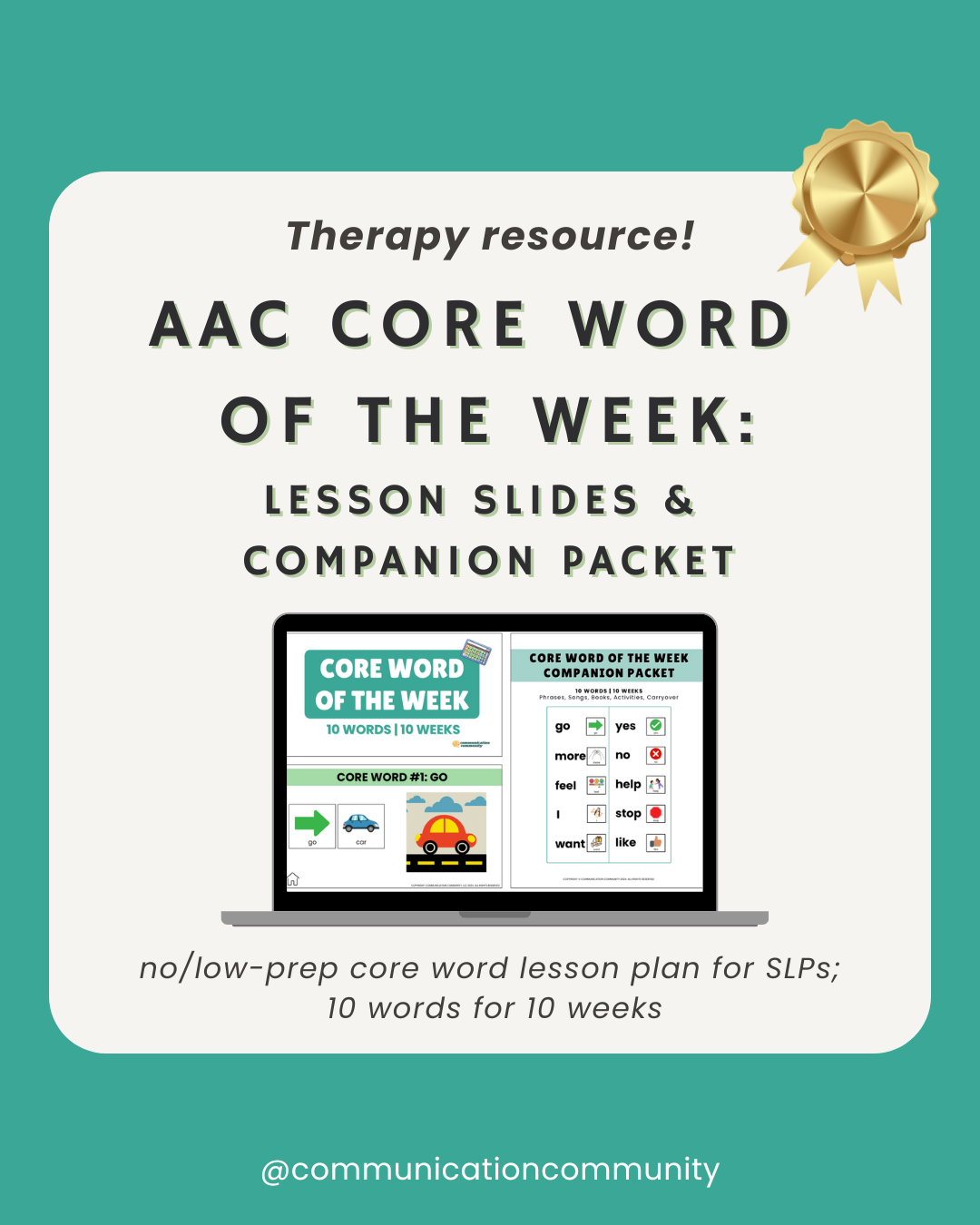
- Core Words
- Fringe Words, Choosing Fringe Words
- Using AAC devices in different contexts/environments
- Partner Training in AAC
Activities using AAC devices:
AAC goals:
Citations/further resources
https://www.speaktome.co.nz/article/augmentative-alternative-and-communication-aac-myths
https://www.asha.org/PRPSpecificTopic.aspx?folderid=8589942773§ion=Key_Issues